The RxSight® Light Adjustable Lens™ (LAL) is the first and only FDA-approved intraocular lens that can be customized to your specific visual needs after cataract surgery.
Customized results
The Light Adjustable Lens (LAL) offers unparalleled flexibility by allowing post-surgical adjustments to fine-tune vision to the patient’s needs. This revolutionary lens can be modified with UV light after implantation, ensuring patients achieve optimal visual clarity that can be customized even after surgery. Dr. Manusis can preview and adjust your vision to your own personal visual requirements after the lens has been implanted.

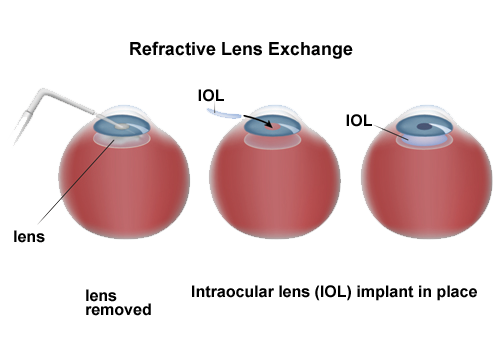
Cataract surgery involves the removal of the cloudy natural lens and replacement with an artificial lens implant. It is one of the most common and successful procedures performed worldwide, helping millions of people restore clear vision. Thanks to continuous advancements in technology and techniques, the field of cataract surgery has evolved significantly in recent years. These innovations in cataract surgery not only enhance the precision and safety of the procedure but also improve visual outcomes and the overall patient experience. Cataracts, once removed, do not recur.
Everyone gets cataracts as we age. Cataract surgery is recommended for individuals experiencing blurry vision, glare, or difficulty with tasks like reading or driving due to cataracts. It’s ideal for patients who want to regain independence and quality of life by eliminating visual limitations.
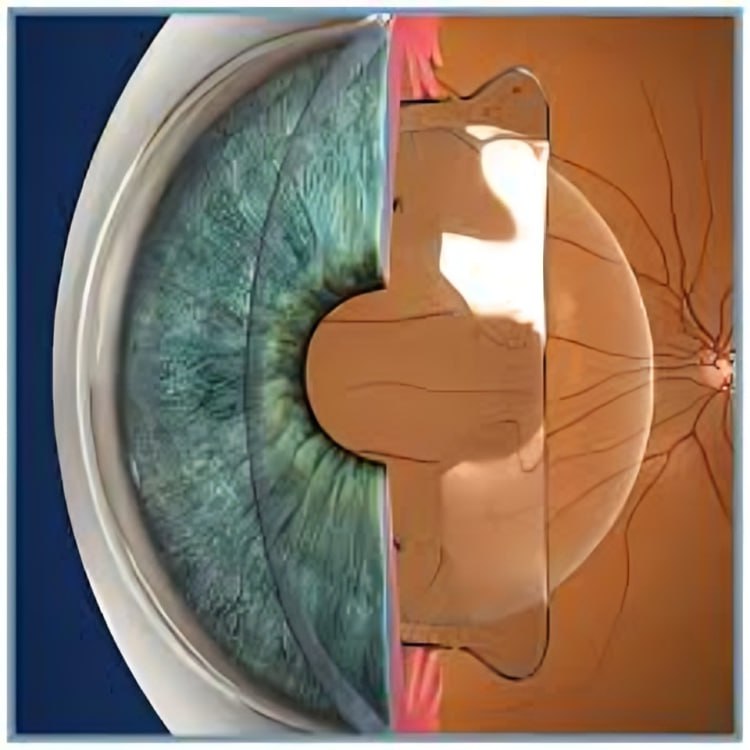
The process begins with a thorough eye examination to assess the extent of cataract development. Dr. Manusis then assists with the intraocular lens selection process to improve vision and reduce dependence on glasses. Intraocular lens selection depends on the overall health of the eye as well as the patient's daily visual needs. Making the right decision is crucial as the implants are there for life. The surgery is then performed in the ambulatory surgery setting. It usually takes about 15-30 minutes with light sedation. Patients can expect a smooth recovery with minimal downtime or discomfort.
Cataract surgery is recommended when vision impairment starts to interfere with everyday tasks such as driving, reading, or recognizing faces. If vision difficulties affect your quality of life, it’s time to consult an eye specialist about surgical options.
Laser-assisted cataract surgery uses advanced laser technology to create precise incisions and soften the cloudy lens for easier removal. This technique enhances accuracy and customization, leading to improved outcomes and faster recovery.
After cataract surgery, mild discomfort, light sensitivity, or itching is normal. Most patients notice significant vision improvement within a day, with continued progress over the following weeks. Key recovery tips include:
Cataract surgery is generally covered by insurance, including Medicare, as a medically necessary procedure. Standard IOLs are typically included, but premium lens options may require out-of-pocket costs. It’s advisable to check with your insurance provider for specific coverage details.
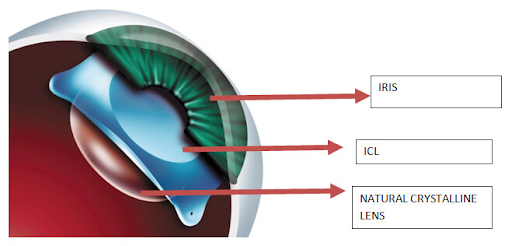
Whether you need glasses after cataract surgery depends on the type of intraocular lens (IOL) used. Standard monofocal IOLs correct vision at a single distance, so glasses may still be needed for near or far vision.
Premium IOLs can address refractive errors such as nearsightedness, farsightedness, astigmatism, and presbyopia, reducing the need for glasses.
Your doctor can help determine the best IOL option based on your vision needs.
Selecting a skilled and experienced surgeon is crucial for optimal cataract surgery outcomes. Factors to consider include:
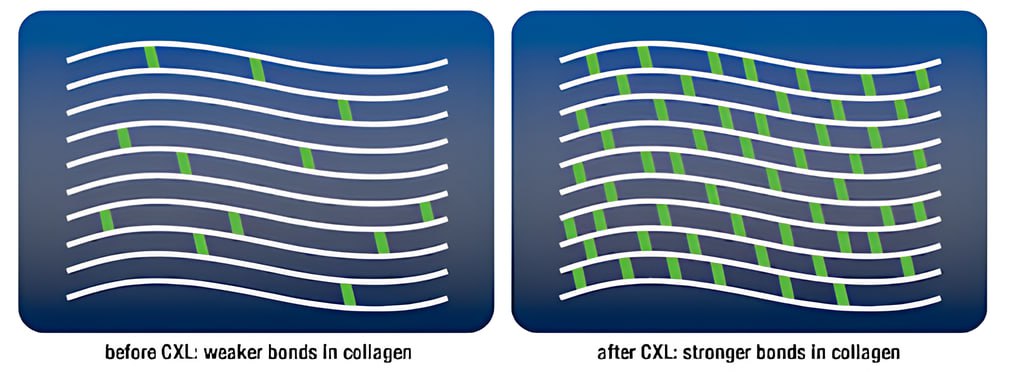
Corneal cross-linking is a surgical procedure aimed at:
What does the procedure involve?
Riboflavin (Vitamin B2) is applied to the eye every 5 minutes for 30 minutes, and then the cornea is illuminated with UV-A light for approx. 10 – 30 minutes. The eye is covered with a bandage contact lens which is removed 5 to 7 days after the procedure. The cornea will be examined and scanned at frequent intervals to monitor for its stability.
Signs you may have dry eye syndrome include:
Allergies
Seasonal or environmental allergies (like pet dander) cause eye dryness and redness.
Medications
Medicines like antidepressants, antihistamines, decongestants and oral contraceptives can reduce your tear production.
Blepharitis
Blepharitis is an inflammatory condition of eyelid margins associated with meibomian gland dysfunction and poor lipid production resulting in premature tear film evaporation and dry eye.
Diabetes
People with diabetes have decreased corneal sensation and therefore do not produce enough tears to provide an adequate tear film.
Autoimmune diseases
Refractive surgery
It is now established that post-LASIK patients will experience dry eyes in the short term. Once corneal nerves repopulate, dry eye symptoms typically improve.
Contact Lenses
Long-term use of contact lenses decreases sensation, especially when worn overnight. Various treatment options are available to ensure comfortable long-term contact lens tolerance.
Eye fatigue
Long-term computer use and reading both have one thing in common — a reduced rate of blinking. After a while, the eyes feel fatigued, and vision blurs due to increasing dryness.
Environment
Airplanes, sitting near air-conditioners, prolonged use of computers, or forced air heating, driving a car, and lack of sleep all can cause dry eye symptoms.
Dry eyes also have dietary components. Increasing water intake and decreasing caffeine and alcohol consumption will most likely improve tear film.
Eyelid disorders
Poor eyelid closure, sleeping with eyes partially open, or having a poor blinking reflex can lead to eye exposure and dryness.
Age
People older than 50 are at a higher risk for dry eye. Tear production and meibum (oil) production decline with age.
Sex
Women are more likely than men to have dry eye due to fluctuating hormones, especially during pregnancy and menopause.
Smoking
Smoking and exposure to second-hand smoke increase your risk of eye irritation and dryness.
Vitamin A and Omega-3 Deficiency
Low levels of vitamin A or Omega-3 fatty acids can contribute to dry eye syndrome.
Autologous Serum Eye Drops
Serum eye drops come from the patient’s own blood serum. They resemble natural tears and contain critical biological factors that can help treat dry eye disease.
Eyelid Thermal Treatment (TearCare®):
TearCare is an eyelid thermal treatment that combines localized heat therapy with manual compression of the eyelids. It treats meibomian gland dysfunction and improves oil production.
Medicated Eye Drops
Your provider may prescribe eye drops that help your eyes increase tear production.
Ointment
Medicated ointment helps to reduce inflammation on the surface of your eyes.
Special contact lenses
Special contact lenses can help treat ocular surface diseases, including dry eye disease.
Tear Duct Blocking
Small silicone plugs are placed in your tear ducts to slow the drainage of your tears. This helps your eyes retain more moisture and helps the tear film better lubricate your eyes.
BlephEx
A special medicated brush cleans eyelids to remove debris and bacterial toxins.
More info can be found at: Dry Eye Statistics

Surgical solution to correct refractive errors and eliminate cataract risk long term by replacing the eye’s natural lens with a custom intraocular implant.
.png)
Surgery offers bladeless cuts, improving accuracy in removing a cloudy lens for a clearer artificial one.